Best Clinic for Pulmonary Embolism Treatment
A Pulmonary embolism Thrombolysis is a blood clot that forms in a vein, travels through your blood and lodges in lungs. A pulmonary embolism is a medical emergency as a result of out sized embolism or sometimes many repeated smaller ones, will be fatal in a short time. Normally, blood flows from the right side of heart to the lungs, where it picks up oxygen.
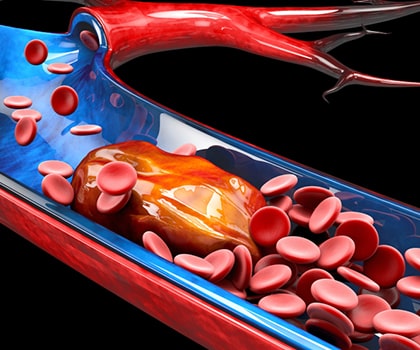
The left side of the heart then pumps this oxygen-rich blood through an arrangement of blood vessels called arteries. Once the blood has delivered the oxygen to different parts of the body, it enters another network of blood vessels known as veins. Veins carry the now oxygen-poor blood back to the heart, which pumps blood to the lungs to pick up oxygen again. If a blood clot forms in a vein, commonly a deep vein in the leg, it can move with the blood flow back to your lungs and lodge there. This blood clot is called a pulmonary embolism.
A patient may experience High Blood Pressure in the lungs, if lung arteries get blocked by a blood clot. As a result, the heart pumps tougher than usual. When the heart is regularly overworked, it may enlarge, and it may eventually fail to perform. Thus, a large pulmonary embolism may result in heart stops functioning. Fortunately, the possibility of living a pulmonary embolism increases once your physician can diagnose and treat the condition quickly.
The symptoms you feel can depend on the site and size of your blood clot. Shortness of breath is the most common symptom. Other symptoms include.
- Rapid breathing;
- Anxiety and restlessness;
- Chest pain, which might extend into your shoulder, arm, neck, and jaw;
- Coughing or spitting up blood;
- Feeling lightheaded or fainting;
- Having a rapid heartbeat.
MEDICAL MANAGEMENT:
If you’ve got a pulmonary embolism, your physician or vascular surgeon may administer an anticoagulant drug called heparin intravenously as initial treatment. Anticoagulants are sometimes called blood thinners. They don’t thin your blood, but they help prevent your blood from clotting too easily. Heparin helps prevent clots from forming and keeps clots you already have from growing.
Eventually, your body breaks up the clot that has caused your pulmonary embolism. Otherwise, a type of medication, called fractionated heparin, may be delivered once or twice daily through an injection in your abdomen. These functions in a very similar fashion to heparin delivered directly into the vein.
INTERVENTIONAL MANAGEMENT- THROMBOLYSIS
If you’ve got an outsized pulmonary embolism or you have another medical condition, your physician may recommend more aggressive treatments. A treatment called thrombolysis can dissolve your clot. In this process, your vascular surgeon injects clot-dissolving drugs through a catheter directly into the clot. Vascular Surgeon inserts a long, thin tube called Catheter into a puncture in the skin over blood vessels. Pulmonary Embolism Thrombolysis has a higher risk for bleeding complications and stroke than anticoagulant therapy but may be effective more quickly, a feature that may be important if the pulmonary embolism is large.
If you’re unable to receive anticoagulant therapy or thrombolysis, your vascular surgeon may attempt to remove the clot using a catheter technique. Using this method called suction Thrombectomy, your physician guides a catheter through your blood vessels to your Pulmonary Embolism Thrombolysis. The Catheter that is inserted into the skin sends a salt solution into the blocked artery. The water pressure pulls the clot toward the tip of the catheter and breaks up the clot. Your vascular surgeon may, as another option, use a catheter attached to a mechanical device such as a rotating head to break up a clot.
Rarely, physicians recommend surgery for a pulmonary embolism. The procedure is called pulmonary Embolectomy. You may need this surgery if you have life-threatening blockages in your lungs that are not responsive to other treatments. Your vascular surgeon will counsel you about the best treatment option for your particular circumstances. Once your pulmonary embolism has been treated, you will usually need to take an anticoagulant drug called warfarin (Coumadin®) for six months or longer to lessen the risk of developing another pulmonary embolism. During the time you are taking medication, your physician will order blood tests to make sure your blood anticoagulation level is adequate to prevent clots but not so high as to cause excessive bleeding. Anticoagulants can cause bleeding problems if the dosage is too high so it is important to follow your physician’s recommendations for testing and dose adjustments.
In some circumstances, your doctor may recommend placement of a special metal filter in your main vein, the vena cava, if drug therapy isn’t feasible or isn’t enough to prevent pulmonary embolisms from recurring. This device is called a vena cava filter. Vena Cava, which is a vein in the abdomen, carries the blood back to the heart and also lungs. Vena cava filters can trap the clots that break away from your leg veins before they can reach your lungs. Vascular Surgeon inserts a Catheter that makes filter into Vena Cava. Some of these filters are left in place enduringly and some can be removed. Your vascular surgeon will advise you regarding what is the best option for your particular situation.
To be effective, the therapy needs to be initiated immediately before permanent damage has occurred. The length of a treatment session varies depending on the underlying cause. A session can take from 60 minutes to 48 hours.
Q: What are the tests needed?
- Chest x-ray
- Electrocardiography (ECG) which measures your heart’s electrical activity
- D-dimer enzyme-linked immunosorbent assay
- Lung scanning, which measures blood flow in lungs and air intake’
- Spiral Computed Tomography (CT) scan
- Pulmonary Angiography, which shows X-ray pictures of the blood vessels in your lungs.
- A duplex ultrasound, which allows your physician to measure the speed of blood flow and to see the structure of your leg veins.
- Venography, which shows x-ray pictures of your leg veins